 |
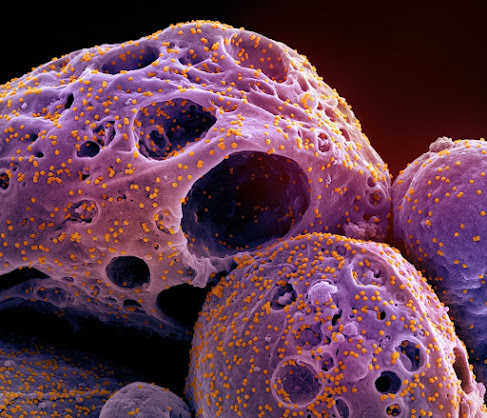
| A new study shows how carrying the biggest genetic risk factor for Alzheimer's disease, the APOE4 gene variant, contributes to disease pathology. Here, black gold staining in postmortem brain tissue shows people with two copies of the APOE3 variant have much more myelin insulation of their neurons than people (bottom row) with a copy of APOE4. Resized Image using AI by SFLORG Image Credit: Tsai Lab/The Picower Institute |
It’s well-known that carrying one copy of the APOE4 gene variant increases one’s risk for Alzheimer’s disease threefold and two copies about tenfold, but the fundamental reasons why, and what can be done to help patients, remain largely unknown. A study published by an MIT-based team in the journal Nature provides some new answers as part of a broader line of research that has demonstrated APOE4’s consequences, cell-type-by-cell-type, in the brain.
The new study combines evidence from postmortem human brains, lab-based human brain cell cultures, and Alzheimer’s model mice to show that when people have one or two copies of APOE4, rather than the more common and risk-neutral APOE3 version, cells called oligodendrocytes mismanage cholesterol, failing to transport the fat molecule to wrap the long vine-like axon “wiring” that neurons project to make brain circuit connections. Deficiency of this fatty insulation, called myelin, may be a significant contributor to the pathology and symptoms of Alzheimer’s disease because without proper myelination, communications among neurons are degraded.

.jpg)

.jpg)


.jpg)

.jpg)





.jpg)
