 |
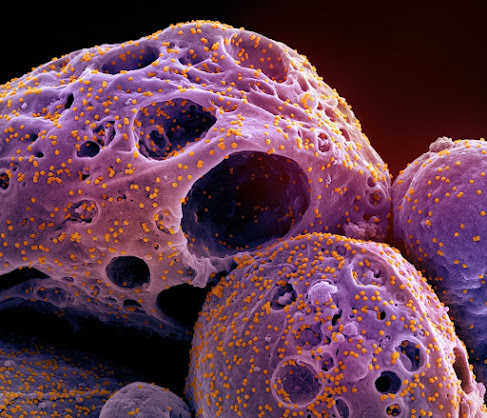
| Monkeypox Virus Illustration Credit: Samuel F. Johanns |
The three antiviral drugs commonly used to treat mpox viruses (monkeypox viruses) are also effective against the viruses from the current outbreak. This has been shown in cell culture experiments by scientists at Goethe University Frankfurt/University Hospital Frankfurt and the University of Kent in Canterbury, Great Britain.
The mpox virus is closely related to the smallpox virus (variola virus), which caused large, deadly outbreaks before it was eradicated by vaccination at the end of the 1970s. While the smallpox virus led to very severe disease progression with a death rate of about 30 percent, mpox is milder. Nevertheless, the mortality rate is still about three percent. Particularly at risk of a severe course of the disease are people with a weakened immune system, elderly persons, pregnant women, newborn babies and young children. Until recently, mpox outbreaks only occurred in certain parts of Africa when humans became infected through contact with wild animals, typically rodents such as the Gambian pouched rat and the rope squirrel.
However, in May 2022 a first large mpox outbreak outside Africa was detected; the virus spread solely through human-to-human transmission. This ongoing outbreak has so far reached more than 100 countries and been classified by the World Health Organization (WHO) as a "Public Health Emergency of International Concern".

.jpg)


.jpg)
.jpg)


.jpg)





.jpg)


.jpg)
.jpg)




.jpg)
