 |
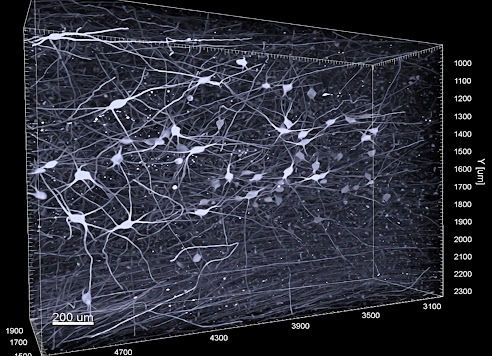
| A section of a brain organoid made from stem cells of a human. In magenta are actively proliferating brain stem cells, in yellow a subset of brain stem cells. Photo Credit: Jan Fischer |
ARHGAP11B - this complex name is given to a gene that is unique to humans and plays an essential role in the development of the neocortex. The neocortex is the part of the brain to which we owe our high mental abilities. A team of researchers from the German Primate Center (DPZ) - Leibniz Institute for Primate Research in Göttingen, the Max Planck Institute for Molecular Cell Biology and Genetics (MPI-CBG) in Dresden, and the Hector Institute for Translational Brain Research (HITBR) in Mannheim has investigated the importance of ARHGAP11B in neocortex development during human evolution.
To do this, the team introduced for the first time a gene that exists only in humans into laboratory-grown brain organoids from our closest living relatives, chimpanzees. In the chimpanzee brain organoid, the ARHGAP11B gene led to an increase in brain stem cells relevant to brain growth and an increase in those neurons that play a critical role in the extraordinary mental abilities of humans. If, on the other hand, the ARHGAP11B gene was switched off in human brain organoids, the quantity of these brain stem cells fell to the level of a chimpanzee. Thus, the research team was able to show that the ARGHAP11B gene played a crucial role in the evolution of the brain from our ancestors to modern humans.























.jpg)
